Epibulbar
dermoid is a choristoma. It is composed of fibrous and fatty tissue,
covered by keratinized epithelium. It is present from birth. A few produce a
lipoid infiltration of the corneal or scleral stroma at their leading edge. In
some instances there may also be subconjunctival dermolipomas (adipose tissue
and dense connective tissue) which are present in the lateral quadrant of the
eye. These can be up to 10 mm in diameter and usually straddle the limbus. Most
are on the inferior temporal limbus1,2. The pathogenesis of
dermoids is multifactorial. Very rarely more than one family members have been
found to have similar lesions3. On
histopathological examination, they contain many tissues including skin, hair, fat, sweat gland, connective
tissue, lacrimal gland, muscle, bone, teeth, cartilage, vascular/neurologic
tissue and may even contain brain tissue. Lymphoid
elements can also be present.
Dermoids are classified into three types on the basis of
location of the lesion. The most common involves the limbus. Limbal dermoids
mostly present as superficial lesions but deeper ocular structures can also be
involved. The second type is entirely in the superficial cornea. The last variety
of dermoid is rare and affects full thickness of cornea and deeper tissue are
replaced with a fibrous and fatty tissue.
Epibulbar Dermoid is often seen
with Goldenhar (oculoauriculovertebral) syndrome4. These patients
may have a variety of other anomalies, including ear deformities (partially
formed ear - microtia or totally absent ear - anotia), preauricular appendages, auricular fistulae, maxillary
or mandibular hypoplasia, vertebral deformities, hemifacial microsomia and vertebral anomalies. Dermoids can be
associated with ocular abnormalities including colobomata of the eyelids, Duane
retraction syndrome and other ocular motility disorders, lacrimal anomalies,
scleral and corneal staphylomata, aniridia, and microphthalmia. Variant
of the syndrome like a fibroepithelial polyp attached to limbal dermoid has
also been described5. Unilateral morning glory syndrome has been
found in a patient with multiple limbal dermoids6. Associations like SCALP7,8 and Nager syndrome9
are reported in the literature. A new grading system keeping in view area of
cornea and conjunctiva involved as well as surface shape has been proposed10.
Reviewing Pakistani literature on the subject found a few case reports and
small studies11–15. This study was carried out to analyze our
experience regarding the clinical presentation and results of simple excision
of limbal dermoids type one in Pakistani population.
MATERIAL
AND METHODS
A total of 15 epibulbar
dermoids presented in oculoplastic and pediatric ophthalmology division of Mughal
eye hospital Lahore and were surgically managed from 1st June 2016 to 30 Dec
2017. This study was approved by the Ethics
Committee of Mughal Eye Hospital and followed the tenets of the Declaration of
Helsinki. Written informed consent was taken from all patients. All the
patients presenting with Type one limbal dermoid (i.e. present at the limbus)
who were concerned about cosmetic appearance and were willing for surgical
removal were included in the study. One case of dermoid which was involving the
entire cornea was excluded. Informed consent was taken from all the participants.
All the excisions were done by the first author. Adults were operated under
local anesthesia and children were operated under general anesthesia. After
excision with blade and scissors, conjunctiva was stitched in 6 (40 %) cases
when lesion was affecting significant part of conjunctiva. All the operated
cases were reviewed in outpatient department on 1st post-operative
day, every week for three weeks and then every month for 4 months. Follow up
ranged from 3 weeks to 4 months (Mean= 6 ± 3.5 weeks).
RESULTS
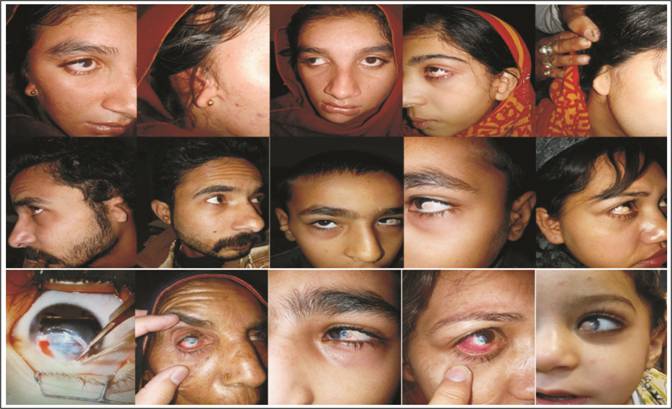
Age ranged from 4 years to 60
years (Mean 18+ 13.48). 3 (20%) out of 15
patients presented in 1st decade of life, 8 (53%) were in second, 3 (20%)
in third decade and one (6.7%) patient in 6th decade of life. All patients
presented due to cosmetic concerns though 12 cases (80 %) had visual
deterioration.
Male to
female ratio was 6:9. All the patients had unilateral epibulbar dermoids. In our study all the patients presented with
epibulbar dermoid in inferior temporal quadrant however in 3 patients (20%)
lesion was more towards inferior aspect of limbus. Most (9
cases - 60%) were present at limbus equally involving cornea and sclera.
However, 3 cases (20%) extended more on the scleral side while 3 cases (20%)
were predominantly on the corneal side. Most (12 cases- 80%) were round and 3
cases (20%) tapering. 5 (33%) had Goldenhar Syndrome (Table 1). 4 (27%) patients
Table 1: Systemic associations of Limbal
Dermoid (Total No. of patients =15).
|
Ocular
& Systemic associations
|
5 (33%)
|
|
Preauricular skin tags
|
4 (27%)
|
|
Ear
deformity
|
3 (20%)
|
|
Maxillary
Hypoplasia
|
1 (7%)
|
|
Divergent
Squint
|
1 (7%)
|
had preauricular tags. Pre
auricular tags were on the same side as the lesion in 2 patients, on opposite
side in 1 patient and bilateral in one patient. One (7%) patient had maxillary
hypoplasia. She also had divergent squint. Postoperatively (Table 2) one
patient (7%) had extensive formation of granulation tissue while one patient
(7%) had corneal thinning and his post-operative steroids were stopped
immediately.
Table 2: Post operative complications.
|
Post
operative complications
|
2 (14%)
|
|
Corneal
thinning
|
1 (7%)
|
|
Extensive
formation of granulation tissue
|
1 (7%)
|
There
was variable yellowish to brownish pigmentation of the lesion in 12 cases
(80%). Five patients (33%) out
of 15 had more marked superficial pigmentation of epibulbar dermoid. Three
(20%) patients had ear deformity (hypoplastic ear - microtia). After excision
cornea and conjunctiva healed within 5-7 days, generally with some scarring and
imperfect corneal transparency; however, the appearance was considerably
improved.
DISCUSSION
Limbal dermoids belong to benign congenital tumors containing
choristomatous tissue i.e. normal tissue derived from germ cells layers, which
is foreign for that site. There is no racial predisposition and males and
females are equally affected. In our study male to female ratio was 6:9. Most
common site of presentation of limbal dermoid is inferior temporal quadrant of
the corneal limbus. Most of limbal dermoids were equally involving corneal and
scleral sides of limbus while in a few patients lesion was more on corneal side
or scleral side. Epibulbar dermoids are dome shaped, with or without
keratinized surface. Hair follicles and cilia are usually visible. They are
fleshy and can have fine superficial vessels. They usually are not malignant.
Multifactorial pattern of inheritance is well-recognized in limbal dermoids
associated with ocular and systemic findings such as Goldenhar syndrome.
In our study, patients presented at different age groups. The late
presentation in our cases was probably due to socio economic reasons as poor
patients could not afford early treatment. Fourteen (93%)
out of 15 patients presented with superficial epibulbar dermoids while one
patient had deep corneal stromal involvement.
Management of limbal dermoids may be conservative with artificial
lubricants and epilation of offending hair if there is foreign body sensation.
Surgical removal of the lesion can be done in case of cosmetic disfigurement or
if it is causing visual disturbance. Surgical treatment is indicated only when
there is requirement for improving the patient's vision or cosmetic appearance.
Surgical removal of the mass which is above the surface of sclera or cornea is
the preferred method. It is unnecessary to completely remove the deeper lesion
as inadvertent entry inside eyeball is high in case of repeated attempts for
complete excision of the lesion. The exposed sclera is covered with the help of
undermining surrounding conjunctiva and suturing it over exposed surface. In
case of removal of most thickness of cornea or sclera, a patch graft is done to
restore thickness of the wall of eyeball. Amniotic membrane may be stitched in
a single or multiple layers at the site if there is risk of perforation. The
amniotic membrane is sutured to underlying sclera or fibrin-glue adhesive is
used to secure the grafted tissue16,17. Placement of a processed pericardial graft to cover exposed
surface after excision has also been tried18. In all of our study cases, superficial
sclerokeratectomy was done with the help of blade and scissors for excision of
epibulbar dermoid. In cases where the epibulbar dermoid was more on scleral
side the defects was closed with simple suturing of the conjunctiva. One patient
had more deep involvement of corneal stroma with postoperative thinning of the
cornea. His postoperative steroids were stopped immediately. One should remain
vigilant and should have a plan to apply patch if there is impending
perforation. One younger patient operated at the age of 4 years had extensive
formation of postoperative granulation tissue. Such cases may be confused to
have recurrent keloid19. Limbal stem
cell transplantation from the same patient has been found effective20.
Sutureless corneoscleral grafts fixed with fibrin glue are becoming more
popular21. 0.02% Mitomycin C applied for 2 min following the excision has been claimed to
prevent occurrence of pseudopterygium following excision22.
Tattooing of the cornea and a conjunctival graft of the same patient after
simple excision has been claimed to produce better postoperative appearance23,24.
Cosmetic concern remains the main indication for the decision to remove limbal
dermoids25. Our study has a few limitations which include relatively
small number of cases, short follow up (as most patients were satisfied and did
not report for follow up) and not using Mitomycin or amniotic membrane so we
cannot comment which is a relatively better procedure. Strength of our study is
that we have preoperative and postoperative photograph of each patient with all
findings. We achieved satisfactory results by simple surgical removal.
CONCLUSION
In our study there was yellowish
to brownish superficial pigmentation in epibulbar dermoid in most cases, which
is not reported earlier to the best of our knowledge. Treatment with excision and superficial
sclerokeratectomy without graft gives satisfactory results. No significant
visual threatening complication was encountered.
Author’s
Affiliation
Dr. Khawaja Khalid Shoaib
FCPS, FRCS, MCPS HPE
Health Bridge Hospital, Ghazi Road,
Near Bhatta Chowk, DHA, Lahore.
Dr. Tariq Shakoor
MCPS, FCPS
Rahbar Medical & Dental
College, Lahore
Dr. Muhammad Shahbaz Amin
MCPS, FCPS
Lahore Medical & Dental
College, Lahore.
Role of
Authors
Dr. Khawaja Khalid Shoaib
Performed Surgery, Review of literature, Collection of Data,
Analysis of Data, Writing Manuscript, Critical Proof reading
Dr. Tariq Shakoor
Review of literature, Collection of Data, Analysis of Data,
Writing Manuscript, Critical Proof reading
Dr. Muhammad Shahbaz Amin
Review of literature, Collection of Data, Analysis of Data,
Writing Manuscript, Critical Proof reading
REFERENCES
1.
Fard AM,
Pourafkari L. Images in clinical medicine. The hairy eyeball—limbal
dermoid. N Engl J Med. 2013; 368 (1):
64.
2.
Dey R, Dey S. Images in clinical medicine. Limbal dermoid. N Engl J Med. 2011; 364 (6):
e9.
3.
Zhu J, Cheng HB,
Fan N, Liu CM,
Yu WH, Chen XM,
Liu XY. Studies of a pedigree with limbal dermoid
cyst. Int J Ophthalmol. 2012; 5 (5):
641-3.
4.
Hafidi Z,
Daoudi R. Limbal dermoid in Goldenhar syndrome. Pan Afr Med J. 2013; 15: 69.
5.
Seymenoğlu G,
Başer E,
Tansuğ N,
Demireli P. An unusual association of Goldenhar syndrome. Int Ophthalmol. 2013; 33 (1): 91-4.
6.
Lowry EA,
de Alba Campomanes
AG. Unilateral
Morning Glory Disc Anomaly With Ipsilateral Limbal Dermoids. J Pediatr
Ophthalmol Strabismus. 2014; 51 Online: e37-9.
7.
Lam J, Dohil MA,
Eichenfield LF, Cunningham BB. SCALP syndrome: sebaceous nevus syndrome, CNS
malformations, aplasia cutis congenita, limbal dermoid, and pigmented nevus
(giant congenital melanocytic nevus) with neurocutaneous melanosis: a distinct
syndromic entity. J Am Acad Dermatol. 2008; 58 (5): 884-8.
8.
Hsieh CW,
Wu YH, Lin SP,
Peng CC,
Ho CS. Sebaceous nevus syndrome, central nervous system
malformations, aplasia cutis congenita, limbal dermoid, and pigmented nevus
syndrome. Pediatr Dermatol. 2012; 29 (3): 365-7.
9.
Malik R,
Goel S,
Aggarwal S. Limbal dermoid in Nager acrofacial dysostosis: a
rare case report. Indian J Ophthalmol. 2014; 62 (3): 339-41.
10.
Zhong J,
Deng Y,
Zhang P,
Li S, Huang H,
Wang B,
Zhang H,
Peng L,
Yang R,
Xu J, Yuan J. New Grading System for Limbal Dermoid: A
Retrospective Analysis of 261 Cases over a 10-Year Period. Cornea, 2018;
37 (1): 66-71.
11.
Moin M, Din I, Nazeer A.
Ocular and Periocular dermoid cysts; a clinicopathological study. Biomedica 2005;
21 (2): 113-6.
12.
Kumkum G, Manish J, Prashant K G, Bhawana R. Goldenhar syndrome: airway and anesthetic management – a case report.
J Pak Med Students 2011; 1 (2): 56-9.
13.
Nadeem S, Raza A.
Presentation of ocular and orbital dermoid cysts at Holy Family Hospital Rawalpindi.
Pak J Ophthalmol 2012; 28 (2): 95-8.
14.
Hayat K, Shahzad M, Lin Z, Miao L, Xue S. Case Report Surgical Therapy Of Unusual Congenital Corneal
Fibroma. J Ayub Med Coll Abbottabad, 2010; 22 (1): 180.
15. Kausar A, Zafar SN,
Altaf S, Khan A. Ophthalmic manifestations
of linear nevus sebaceous/organoid nevus syndrome. J Coll Physicians Surg Pak. 2015; 25 (3): 220-2.
16.
Pirouzian A, Ly H, Holz
H, Sudesh RS, Chuck RS. Fibrin-glue assisted multilayered amniotic membrane
transplantation in surgical management of pediatric corneal limbal dermoid: a
novel approach. Graefes Arch Clin Exp Ophthalmol. 2011; 249 (2): 261-5.
17.
Pirouzian A. Management of pediatric corneal limbal dermoids. Clin Ophthalmol. 2013; 7: 607-14.
18.
Lazzaro DR,
Coe R. Repair of limbal dermoid with excision and
placement of a circumlimbal pericardial graft. Eye Contact Lens, 2010;
36 (4): 228-9.
19. Gaviria JG,
Johnson DA,
Scribbick F 3rd. Corneal keloid mimicking a recurrent limbal dermoid. J Pediatr
Ophthalmol Strabismus. 2005; 42 (3): 189-90.
20. Hong S,
Kim EJ,
Seong GJ,
Seo KY. Limbal Stem Cell Transplantation for Limbal Dermoid. Ophthalmic Surg Lasers
Imaging, 2010; 9: 1-2.
21.
Zhou AX,
Ambati BK. Sutureless Lamellar Corneoscleral Patch Graft with Fibrin
Sealant for Limbal Dermoid Removal. J Pediatr Ophthalmol
Strabismus. 2016 Jun. 3; 53 Online: e22-5. Doi:
10.3928/01913913-20160509-03.
22.
Lang SJ,
Böhringer D,
Reinhard T. Surgical management of corneal limbal dermoids:
retrospective study of different techniques and use of Mitomycin C. Eye (Lond). 2014; 28 (7): 857-62.
23.
Jeong J,
Song YJ,
Jung SI,
Kwon JW. New surgical approach for limbal dermoids
in children: simple excision, corneal tattooing, and sutureless
limboconjunctival autograft. Cornea, 2015;
34 (6): 720-3.
24.
Cha DM,
Shin KH,
Kim KH,
Kwon JW. Simple keratectomy and corneal tattooing for limbal
dermoids: results of a 3-year study. Int J Ophthalmol. 2013; 6 (4):
463-6.
25.
Matsuo T. Clinical decision upon resection or observation of
ocular surface dermoid lesions with the visual axis unaffected in pediatric
patients. Springerplus, 2015; 4: 534.